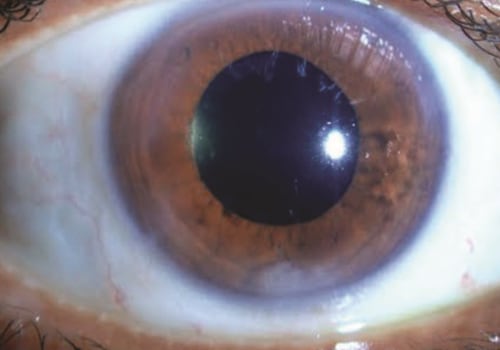
Cataract surgery is a common procedure to remove the lens from the eye and replace it with an artificial lens. It is a safe and effective procedure, but there are some potential complications that can occur. In this article, we will discuss what to look out for after cataract surgery, including signs of posterior capsular opacification (PCO), diphotopsy, and retinal detachment. If there is a progression of pain, decreased vision, or any eye discharge, patients are advised to seek medical attention.
PCO is the most common
long-term complication of cataract surgery
. It can cause “unwanted visual images” after surgery, also known as diphotopsy. Glare, halos, and light streaks are examples of positive dysphotopia. They occur most often at night or in low light, and are more common with multifocal lenses.Residual refractive error can also cause positive dysphotopsia, and the correct prescription of eyeglasses will correct this. If PCO is the culprit, YAG laser treatment may resolve the problem. After the procedure, you usually stay at the doctor's office for about an hour to make sure that your eye pressure doesn't increase. Other complications are rare, but may include increased eye pressure and retinal detachment.
If you have cataracts in both eyes, your doctor usually schedules the second surgery after the first eye has healed. A study of more than 221,000 cataract surgery patients showed that 99.5% of patients had no serious complications after the procedure. Only one laser treatment is required to permanently eliminate vision loss caused by opacification of the back capsule after cataract surgery. In some cases, PCO may occur because some of the old cataract cells are not removed during surgery.
During phacoemulsification, the most common type of cataract surgery, the tip of the ultrasound probe vibrates quickly to emulsify and break up the cataract before it is suctioned by the surgeon (top). Statistics suggest that the lifetime risk of a detached retina as a complication of cataract surgery in the United States is around 1%. If possible, it may be beneficial to evaluate and treat other eye problems before making a decision to undergo cataract surgery. Tell your doctor if you take any medications for prostate problems, as some of these medicines may interfere with cataract surgery.
Sometimes, cataract surgery doesn't improve vision because of underlying eye damage caused by other conditions such as glaucoma or macular degeneration. When complications from cataract surgery occur, most are minor and can be successfully treated by medical means or with additional procedures. Sometimes blurred vision is due to PCO, a fairly common complication that can occur weeks, months or (more often) years after cataract surgery. People whose vision doesn't improve after cataract surgery often have underlying eye disorders such as age-related macular degeneration, diabetic retinopathy or other eye conditions. These are signs of retinal detachment, a rare complication of cataract surgery that occurs when the retina separates from the back of the eye. It is important to be aware of these potential complications so that you can seek medical attention if necessary.